Why Co-Occurring Treatment Matters in Recovery
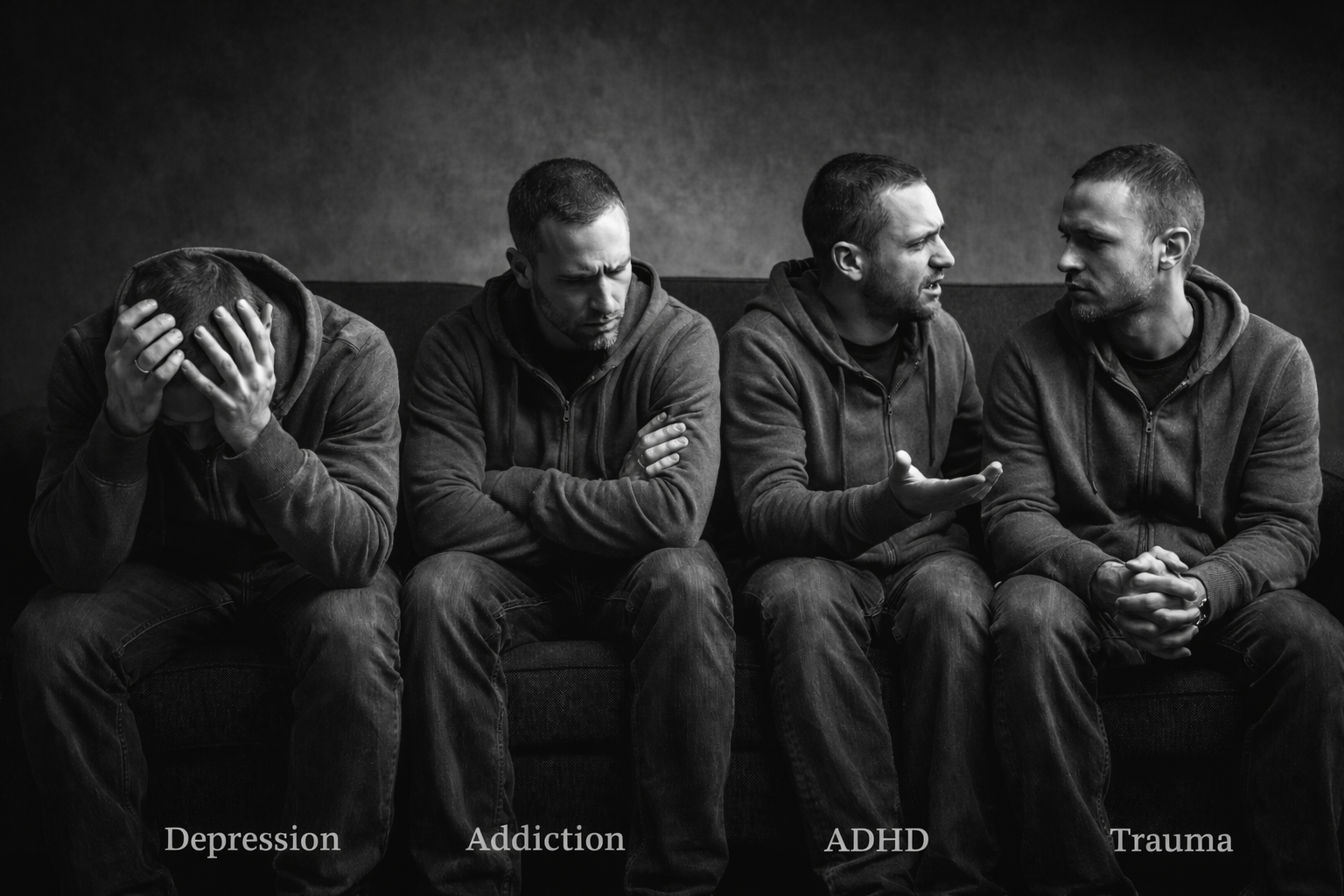
Substance use disorders rarely exist on their own. Research consistently shows that a large percentage of people seeking addiction treatment also live with mental health conditions such as depression, anxiety, trauma-related disorders, ADHD, or bipolar disorder. When these conditions are treated separately or sequentially, outcomes are weaker and relapse risk increases.
Co-occurring treatment, sometimes called integrated treatment, addresses substance use and mental health together, at the same time, within one coordinated plan of care. This approach is widely recognized as the gold standard for effective, long-term recovery.
What the Research Shows
Studies from organizations such as SAMHSA and the National Institute on Drug Abuse show that people with co-occurring disorders have better outcomes when both conditions are treated simultaneously. Integrated care has been linked to:
- Reduced substance use and relapse rates
- Improved mental health stability
- Higher treatment retention
- Better functioning in daily life, work, and relationships
When mental health symptoms go untreated, substances are often used as a form of self-medication. Likewise, untreated substance use can worsen mental health symptoms. Treating only one side of the equation leaves people vulnerable to repeating the same cycle.
Why Integrated Care Works
Co-occurring treatment works because it recognizes how closely mental health and addiction are connected. Trauma can drive substance use. Anxiety can increase cravings. Depression can make recovery feel impossible. ADHD can affect impulse control and follow-through. Addressing these factors together allows treatment to target root causes rather than symptoms alone.
Integrated care also reduces fragmentation. Instead of navigating multiple systems, providers, and treatment philosophies, individuals receive coordinated care that moves in the same direction.
Project Turnabout’s Integrated Clinical Approach
At Project Turnabout, co-occurring treatment is not an add-on. It is built into how care is delivered from the start.
Each individual is supported by a multidisciplinary clinical team that works together throughout treatment. This team may include:
- Licensed Alcohol and Drug Counselors
- Licensed Mental Health Professionals
- Nursing staff with experience in withdrawal management and stabilization
- Psychiatry services, including telemedicine when appropriate
- Admissions and care coordination staff who support continuity across levels of care
Mental health counselors and substance use counselors collaborate closely, ensuring treatment plans reflect both clinical needs and recovery goals. Nursing staff provide medical oversight and stabilization, while psychiatry support helps assess and manage mental health symptoms that may affect recovery.
This team-based approach allows treatment plans to evolve as individuals stabilize, gain insight, and move through different phases of care.
Evidence-Based Therapies, Applied Together
Project Turnabout uses evidence-based practices that are effective for both substance use and mental health, including:
- Cognitive Behavioral Therapy (CBT)
- Dialectical Behavior Therapy–informed care
- Trauma-informed treatment principles
- Relapse prevention planning
- Skills-based education and coping strategies
-
By applying these approaches across disciplines, treatment supports emotional regulation, decision-making, distress tolerance, and long-term behavior change.
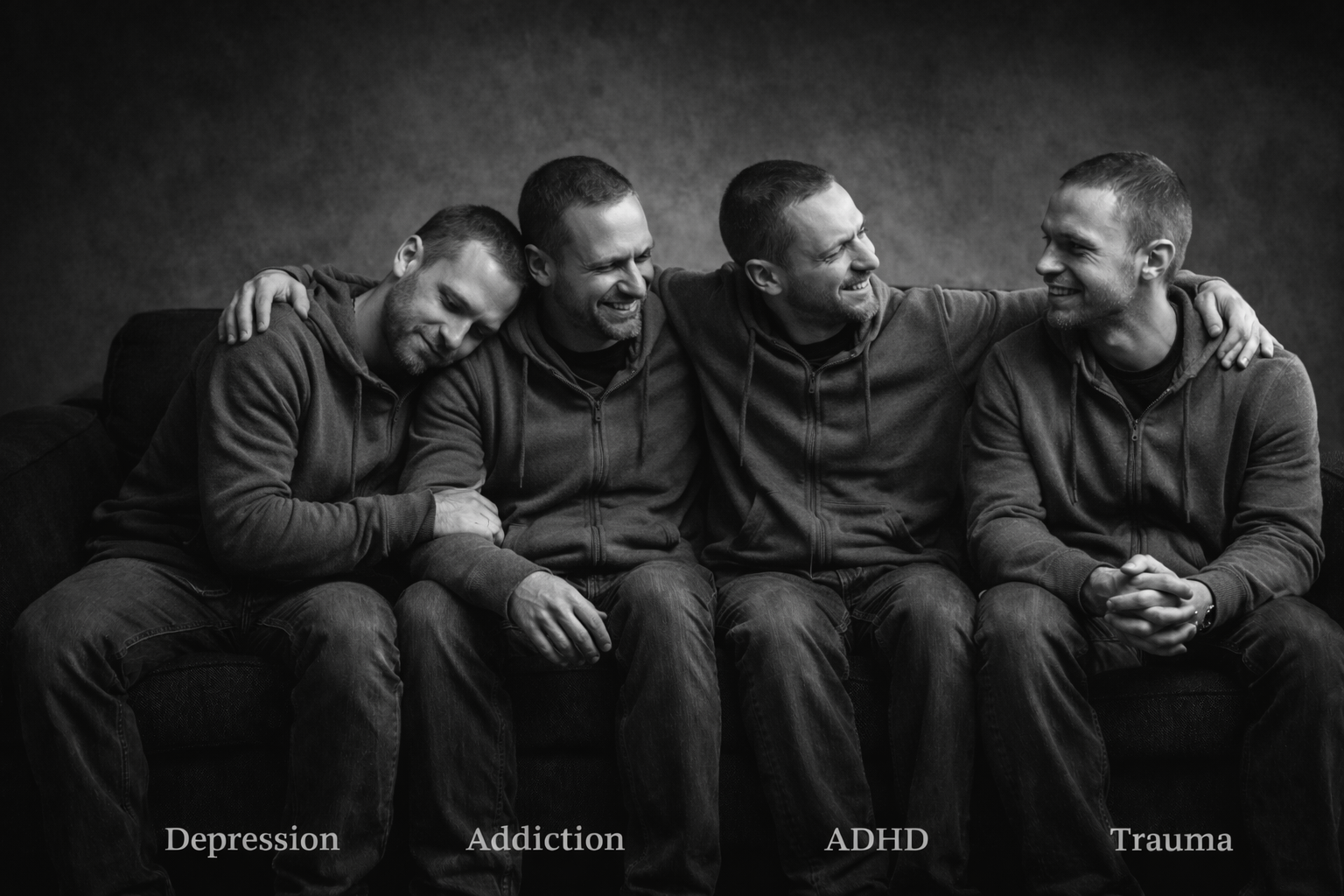
Treating the Whole Person
Recovery is not just about stopping substance use. It is about learning how to live with emotions, stress, relationships, and responsibilities without returning to old patterns. Co-occurring treatment helps individuals understand themselves more clearly, build healthier coping skills, and create a foundation that supports lasting recovery.
At Project Turnabout, integrated care means no one is asked to choose which part of themselves deserves treatment. Mental health and addiction are addressed together, with respect, structure, and clinical integrity.
If you or someone you love is struggling with both substance use and mental health concerns, one conversation can help clarify next steps and determine the right level of care.