Gambling: What is Happening to Me?
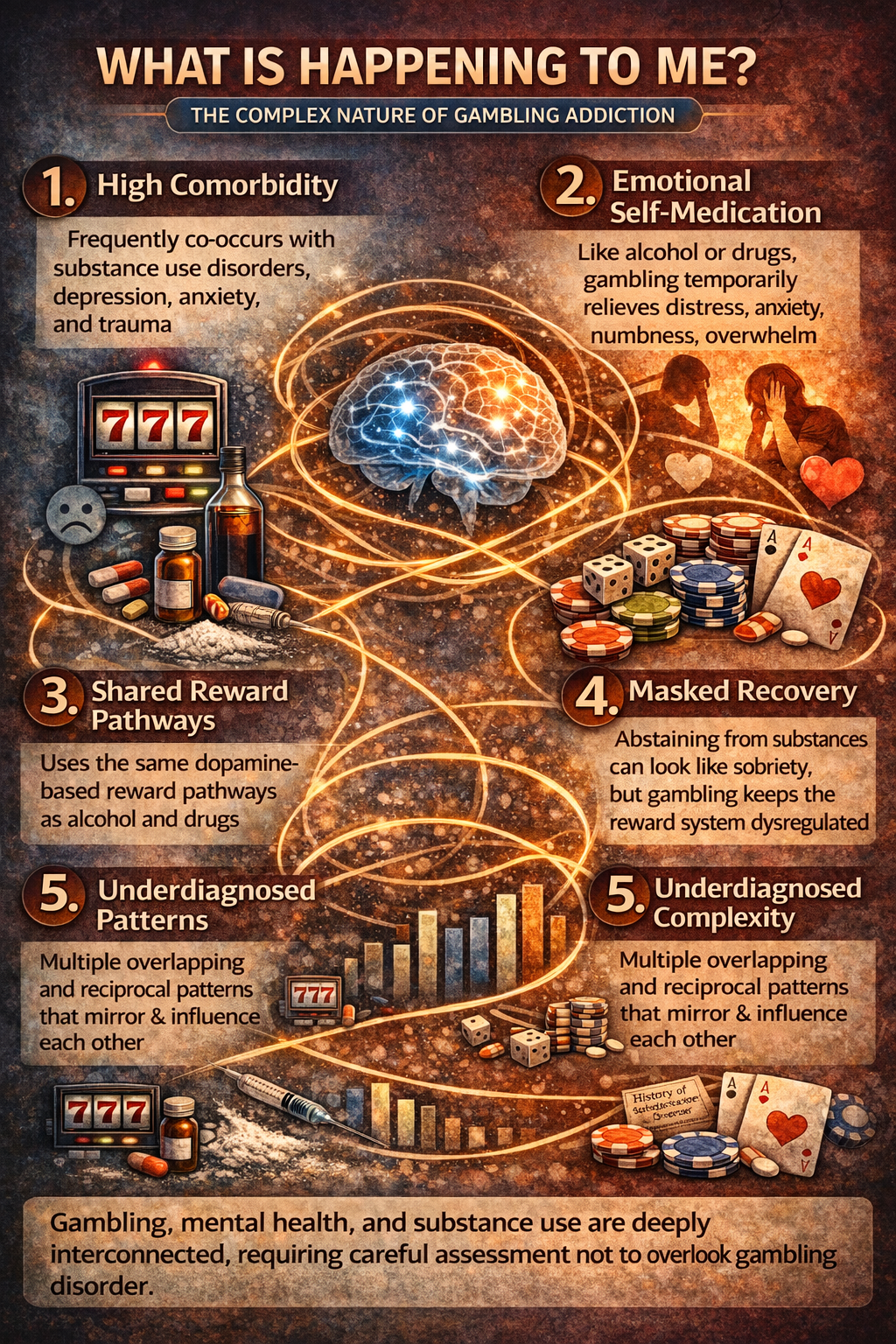
Gambling addiction is often confusing for patients in recovery because it frequently cooccurs with other mental health and substance use disorders, and it can function like a “chameleon” — taking on different psychological roles depending on a person’s underlying vulnerabilities.
Despite growing recognition, gambling disorder remains relatively underresearched and undertreated compared with substance use disorders, and its mechanisms are poorly understood in clinical practice.
1. Gambling Disorder Is Highly Comorbid with Other Addictions and Mental Health Conditions
Decades of epidemiological research show that gambling disorder rarely occurs in isolation. Major studies have found that pathological or problem gambling is strongly associated with other substance use disorders, mood disorders (e.g., depression), and anxiety disorders. In large representative samples, pathological gamblers have substantially higher risks of lifetime alcohol misuse and other substance use disorders compared with nongamblers, and elevated rates of mood and anxiety disorders.
A multiyear longitudinal study also found that the presence of mental health disorders (e.g., anxiety, depression) significantly predicts cooccurring addictive behaviors over time, suggesting these conditions frequently develop alongside or in interaction with gambling problems.
2. Gambling May Serve as a Form of Self-Medication or Emotional Regulation
Many individuals with underlying anxiety or mood symptoms may unconsciously use gambling to relieve emotional distress, much as others selfmedicate with alcohol or drugs. Research on selfmedication in anxiety demonstrates that individuals who engage in selfmedication have a markedly increased risk of developing new substance use disorders; this concept is relevant to gambling too, as gambling can temporarily reduce anxiety or negative affect.
Difficulties with emotion regulation — the ability to manage or process emotions — are strongly linked to pathological gambling, anxiety, depression, and substance abuse. Individuals who struggle with coping skills may be more likely to use gambling to obtain emotional relief.
3. The Brain’s Reward System Does Not Distinguish Gambling from Substance Use
Although gambling does not involve an ingested drug, its psychological and neurobiological effects engage the same reward pathways implicated in substance use disorders (e.g., dopaminergic circuits). This explains why individuals with a history of stimulant use or other dependencies can experience gambling as similarly stimulating or reinforcing, instead of as true “abstinence.” Behavioral neuroscience studies show that repeated exposure to gamblinglike reward schedules can biologically prime the brain in ways that enhance sensitivity to stimulants such as amphetamines, suggesting overlapping neural mechanisms.
4. Cooccurring Disorders Can Obscure Clinical Presentation and Mislead Recovery Assessment
A patient with a history of stimulant use might believe they are sober due to abstaining from meth or cocaine, but if they have engaged in frequent gambling during that period, their core reward system may remain dysregulated. Gambling can thus act as an ongoing stimulantlike behavior, perpetuating addiction pathways and making the individual appear to be in recovery when underlying neural vulnerability persists.
In other words: true remission requires resolution of the maladaptive rewardseeking behavior — not only cessation of substance use. Given gambling’s potent reinforcement, continued gambling in someone with a history of stimulant addiction may indicate that that person’s addictive processes are not in genuine remission.
5. Cooccurring Patterns Are Complex, Reciprocal, and Often Underdiagnosed
Research strongly supports the idea that gambling and other addictive or psychiatric disorders influence each other in complex, reciprocal ways — not as simple causal chains. Some studies indicate that mood and anxiety disorders can precede gambling problems; in other cases, gambling precedes substance use issues or exacerbates existing mental health conditions.
This complexity contributes to diagnostic confusion and misclassification in clinical settings. Without careful assessment of both gambling and other addictive behaviors (e.g., stimulants, alcohol, benzodiazepines), patients are at risk of treatment being targeted at the wrong problem or missing key drivers of their distress entirely

Julie Cunningham
LADC, JD, ICGC - I, Unit Coordinator Vanguard